Living well with Parkinson’s disease
[5 MIN READ]
In this article:
-
Someone in the United States is diagnosed with Parkinson’s disease every nine minutes, according to a recent study from the Parkinson’s Foundation.
-
April is Parkinson’s Awareness Month, dedicated to increased awareness and improved understanding of the chronic condition that affects roughly one million people in the U.S.
-
A movement disorder specialist from Swedish describes how clinical research, new medication and team-based, collaborative care is helping people with Parkinson’s lead active, independent lives.
A recent study from the Parkinson’s Foundation shows that someone in the United States is diagnosed with Parkinson’s disease every nine minutes. And the number of people living with this serious chronic condition is expected to reach 1.2 million by 2030.
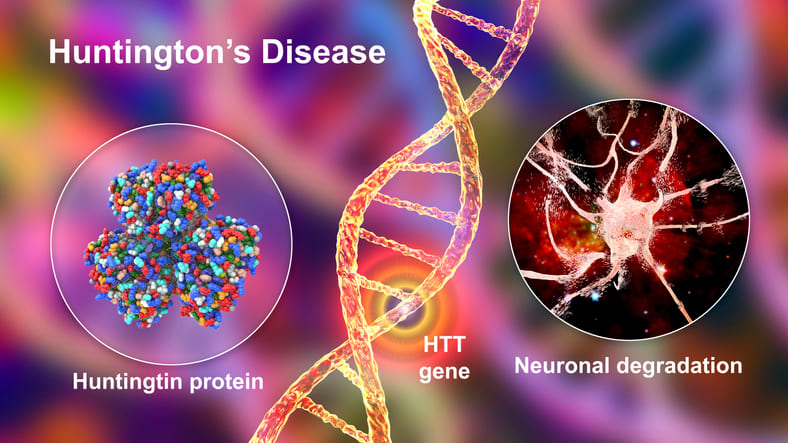
Parkinson’s disease is a movement disorder. It occurs when your brain doesn’t produce enough dopamine, damaging nerve cells and disrupting brain function. There is no cure for Parkinson’s. However, diagnosis, treatment and disease management have improved considerably over the last decade, according to Pravin Khemani, M.D., neurologist at Swedish Neuroscience Institute.
April is Parkinson’s Awareness Month. We talked to Dr. Khemani to get a preview of what’s on the health care horizon for Parkinson’s patients.
“Parkinson’s treatment has entered a promising era of multidisciplinary medical and surgical interventions,” says Dr. Khemani. “Many treatments, therapies and approaches are available to help you manage your condition, minimize symptoms and enjoy a full, healthy and independent life. I’m excited about what the future holds for patients – from new drugs to research breakthroughs.”
Living with a life-changing diagnosis
Parkinson’s is a movement disorder that causes problems called motor symptoms and non-motor symptoms.
Motor symptoms include:
- Tremors and shaking
- Stiffness and slowness
- Soft speech
- Difficulty walking and reduced mobility
- Balance issues
The non-motor symptoms can be even more troubling, according to Dr. Khemani.
“People with Parkinson’s experience cognition and memory issues such as dementia which can significantly interfere with activities of daily living. Some people have behavioral problems leading to hallucinations, delusions and paranoia. In the advanced stages, vision problems and challenges with swallowing and speech are common,” he explains.
Other non-motor symptoms include:
- Irregular blood pressure
- Dizziness, lightheadedness
- Depression and anxiety
- Impaired digestion and poor gut health
- Overly frequent urination and incontinence
- Disrupted sleep
It takes a village
The phrase “multidisciplinary care” is frequently used when discussing health care. But the words represent much more than a marketing slogan when caring for people with Parkinson’s, according to Dr. Khemani.
“Multidisciplinary care involves physicians, medicines, community resources, social services and rehabilitation. We have to build a care plan for the patient that is multifaceted and tailored to their unique needs. This is one of those diseases in which many aspects of the body are involved. No one person has the complete expertise to treat someone with Parkinson’s,” he explains.
That’s why the Movement Disorder Program at Swedish uses a team approach.
“Every person with Parkinson’s needs a dermatological examination because melanomas are at a higher incidence in Parkinson’s than in other diseases,” explains Dr. Khemani. “A person with Parkinson’s needs physical, speech and occupational therapy. If your blood pressure is not good, we work with your primary care doctor. Bladder problems? Then we coordinate with your urologist. If you have cognitive issues, we work with a behavioral health and cognitive specialist. And that’s just a snapshot of what we do to make people live well.”
Treatment varies depending on your illness and health history. Options include:
- Neuro-rehabilitation to develop and implement balance exercises and fall prevention strategies.
- Occupational therapy to help you modify activities, create strategies or identify tools to help you complete activities of daily living, like showering, getting dressed or eating.
- Physical therapy to help minimize the loss of mobility, maintain balance, and remain flexible
- Speech therapy to improve vocal cord function and speech output and strengthen swallowing muscles.
- Medications to help you manage your symptoms.
New treatment, new hope
The standard of treatment for Parkinson’s disease is a medication called Levodopa, which supplements dopamine production. Your body uses dopamine to relay messages between nerve cells. With Parkinson’s, dopamine is reduced because the nerve cells that produce it die off gradually. Levodopa boosts dopamine production and increases the amount available to your brain.
Several new medications developed over the past couple of years have improved the quality of life for people with Parkinson’s. And several more are expected soon, according to Dr. Khemani.
“Two or three new formulations are coming out that we’re excited about,” he explains. “One is an injectable formulation given through a small catheter through the skin, which provides dopamine continuously to the brain. Why is that important? Instead of taking a pill every three to four hours, this provides a continuous dopamine flow to the brain.”
Other advances include:
- Cellular therapies, including stem cells and antibodies, are being studied to reduce brain inflammation, which interferes with the destructive processes that cause the death of brain cells and remove abnormal proteins that cause disease spread from the brain.
- Surgical treatment of Parkinson’s has entered a new era of brain-machine interfacing, which allows surgeons to implant electrodes accurately and providers to program those electrodes more effectively.
- Focused ultrasound is a new treatment that can help reduce Parkinson’s symptoms.
- Genetic therapies address the specific genes that cause Parkinson’s.
“Focused ultrasound (FUS) is a treatment that uses very precisely guided ultrasound waves to cause a lesion that then interrupts and destroys tremor-causing brain cells brain circuitry implicated in Parkinson’s,” says Dr. Khemani.
Currently, FUS is approved for the treatment essential tremor and Parkinson’s disease.
Clinical research for a brighter future
Research studies and clinical trials pave the way for improved care and better quality of life after a Parkinson’s diagnosis. Swedish is currently participating in several active trials to test the effectiveness of new medications for Parkinson’s.
“Tomorrow’s care will be better because of today’s research,” says Dr. Khemani. “Progress requires building rapport and relationships with our colleagues. It requires a lot of elbow grease, not just by the physicians but the clinic staff. Typically, you have to be a university or an endowed center to offer this level of care. Not every facility has knowledgeable people to bring together all these services. We do.”
Learn more and find a provider
The Movement Disorders Program at Swedish offers comprehensive care from providers in many different specialties. This multidisciplinary approach gives you access to innovative and proven treatments based on science and compassion.
Swedish Virtual Care connects you face-to-face with a nurse practitioner who can review your symptoms, provide instruction, and follow up as needed. If you need to find a provider, you can use our provider directory.
Join our Patient and Family Advisory Council.
Related resources
Improved quality of life for patients with essential tremor
Living and thriving with Parkinson’s disease
Voices from the frontline: Ariana Tart-Zelvin, Ph.D., talks about helping dementia patients
This information is not intended as a substitute for professional medical care. Always follow your health care professional’s instructions.